In January 2022, an era of unwavering leadership for the Institute for Safe Medication Practices (ISMP) comes to an end, as Michael R. Cohen, a persistent advocate for medication safety, has stepped down as President of ISMP. Mike will continue to support ISMP’s critical lifesaving work as President Emeritus, and Rita K. Jew, a respected and worthy successor, has been appointed as the new ISMP President (to learn more about Rita, click here).
Mike will continue to be actively involved with ISMP part-time, working on newsletters and special projects close to his heart, continuing his quest for excellence in medication safety. He is an inspiration to us all, and we are delighted that he will continue to be available to ISMP. Rita will lead ISMP into a new era, as ISMP continues to provide sage guidance to influence companies, organizations, practitioners, and consumers who make, regulate, prescribe, dispense, administer, and receive medications, always focusing on the patient.
ISMP roots
As many know, the origin of ISMP is rooted in a monthly column entitled Medication Errors, that began in March 1975 in Hospital Pharmacy. The column grew from a conversation Mike had in 1974 with Neil Davis, both of whom were working at Temple University Hospital in Philadelphia. They were discussing a serious medication error that happened at a local hospital in which a prescriber had used an abbreviation, U for “units,” and a nurse had misread the handwritten U as a zero and administered 40 units of regular insulin to a patient instead of 4 units. The patient developed signs of severe hypoglycemia that required immediate treatment.
Dr. Davis, who was an editor of Hospital Pharmacy, suggested that the incident served as an opportunity for educating other healthcare professionals about this error-prone abbreviation. During the discussion, it became clear that much could be gained by publishing other medication errors that readers may be inclined to report in confidence to prevent patient harm and save lives. Thus, an idea was born and realized to create a national medication error reporting program that practitioners could use to confidentially report medication errors, which could then be shared anonymously with others for learning purposes.
In 1977, Mike began a similar column for nurses in Nursing ‘77, and both the Hospital Pharmacy and Nursing ‘77 columns became leading features in the respective monthly journals. The columns prompted reports of errors from across the US, and Mike would often follow up with the practitioner to learn more about what had happened. Then Mike would share the deidentified error stories and provide error-prevention recommendations in the journal columns so others could proactively take action. Mike and Dr. Davis also began to interact with the US Food and Drug Administration (FDA), USP, The Joint Commission (TJC), and product manufacturers when important issues arose.
By 1990, Mike realized that his advocacy work for safe medication practices and products was a full-time calling that should be supported by a nonprofit organization. Shortly thereafter, ISMP was founded, and by 1994, the organization became the nation’s only 501c (3) nonprofit organization devoted entirely to preventing medication errors. Since then, ISMP has served as a vital force for progress in medication safety through its unyielding advocacy and the development of resources and learning opportunities for healthcare practitioners and consumers.
ISMP’s impact
ISMP has had a tremendously positive impact on patient safety, medication safety, and the practices of caregivers striving to provide quality and safe patient care, both across the US as well as internationally, including through ISMP sister organizations located in Brazil, Canada, and Spain, and as a founding member of the International Medication Safety Network (IMSN).
Along the way, ISMP has cultivated excellent relationships with other patient safety and professional organizations, accreditors, regulators, standards-setting organizations, and the medical products industry that allow us to share our recommendations with organizations so necessary changes can be made to prevent both product- and practice-related medication errors. For example, over the years, ISMP’s frequent interactions with FDA, USP, and the medical products industry have improved the safety of thousands of products, and have had a significant impact on labeling, packaging, and nomenclature guidances and standards. Additionally, ISMP’s collaboration with TJC, the Centers for Disease Control and Prevention (CDC), the Centers for Medicare & Medicaid Services (CMS), professional organizations, and patient safety organizations has resulted in collaborative projects to advance our mutual goal of medication safety, as well as substantial changes in medication safety standards. Likewise, our recommendations to practitioners, healthcare providers, and organizations have also resulted in system- and practice-level changes. In fact, ISMP was among the first, if not the first, organization to recommend the following concepts to improve medication safety, many of which are widely implemented by healthcare providers and industry:
- Free flow protection for infusion pumps
- Removal of potassium chloride injection concentrate from patient care units
- VinCRIStine administration via a minibag instead of a syringe
- Establishing a list of high-alert medications with layered error-reduction strategies
- Use of failure mode and effects analysis (FMEA) in healthcare
- Spotlighting Targeted Medication Safety Best Practices for Hospitals
- Employing a medication safety officer
- Maintaining a look-alike/sound-alike drug name list
- Maintaining a list of error-prone abbreviations that should never be used
- Use of tall man letters
- Calling infusion pumps with a dose error-reduction system (DERS) “smart pumps”
Throughout the years, there have been numerous times when ISMP has also brought together key stakeholders, sometimes for the first time, to discuss complex medication safety issues and create consensus-based best practices and/or action plans for organizations to implement. In some cases, ISMP has been a prickly thorn in the side, provoking important questions, challenging preexisting assumptions, exposing harmful medical products, and chipping away at the resistance to much needed system changes. At other times, ISMP has been a nurturing, healing shoulder to cry on when well-meaning and competent providers have inadvertently harmed a patient—because we are fallible human beings deeply troubled by our inability to “do no harm.”
But perhaps ISMP’s greatest contribution to healthcare has been giving a voice to health professionals who, in confidence, report errors to ISMP for altruistic reasons and/or share their ideas, observations, or questions with ISMP, without fear of even a disparaging thought. ISMP empowers others to give voice to their experiences because they trust ISMP and know their information will be used productively. Every idea, observation, question, or error report ISMP receives is carefully reviewed. Then ISMP healthcare professionals interact internally to apply their collective expertise to arrive at safety recommendations and then share compelling stories about medication errors and impactful change strategies. ISMP aims to draw national attention to medication safety problems, offers healthcare providers new ways of looking at problems, and inspires change.
Excerpted, with permission, from "2022 Ushers in the Beginning of a New Era at ISMP" January 13, 2022 Read on...


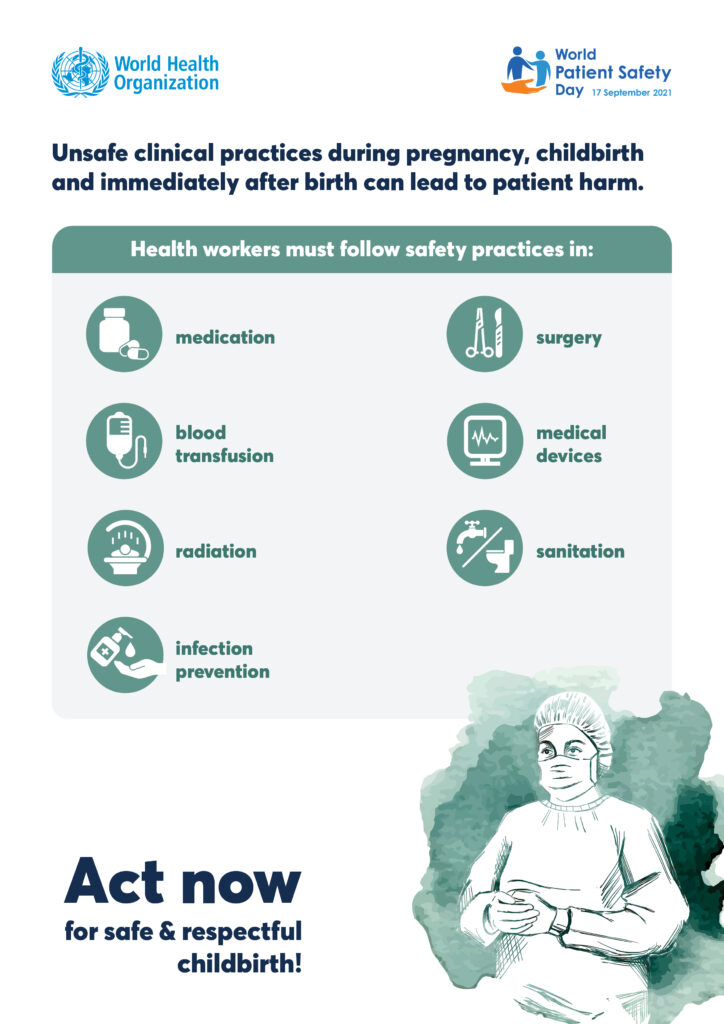
 Many of the resources provided by the International Medication Safety Network (IMSN) are applicable to medication safety during childbirth and the postpartum period for both mothers and newborns.
Many of the resources provided by the International Medication Safety Network (IMSN) are applicable to medication safety during childbirth and the postpartum period for both mothers and newborns.